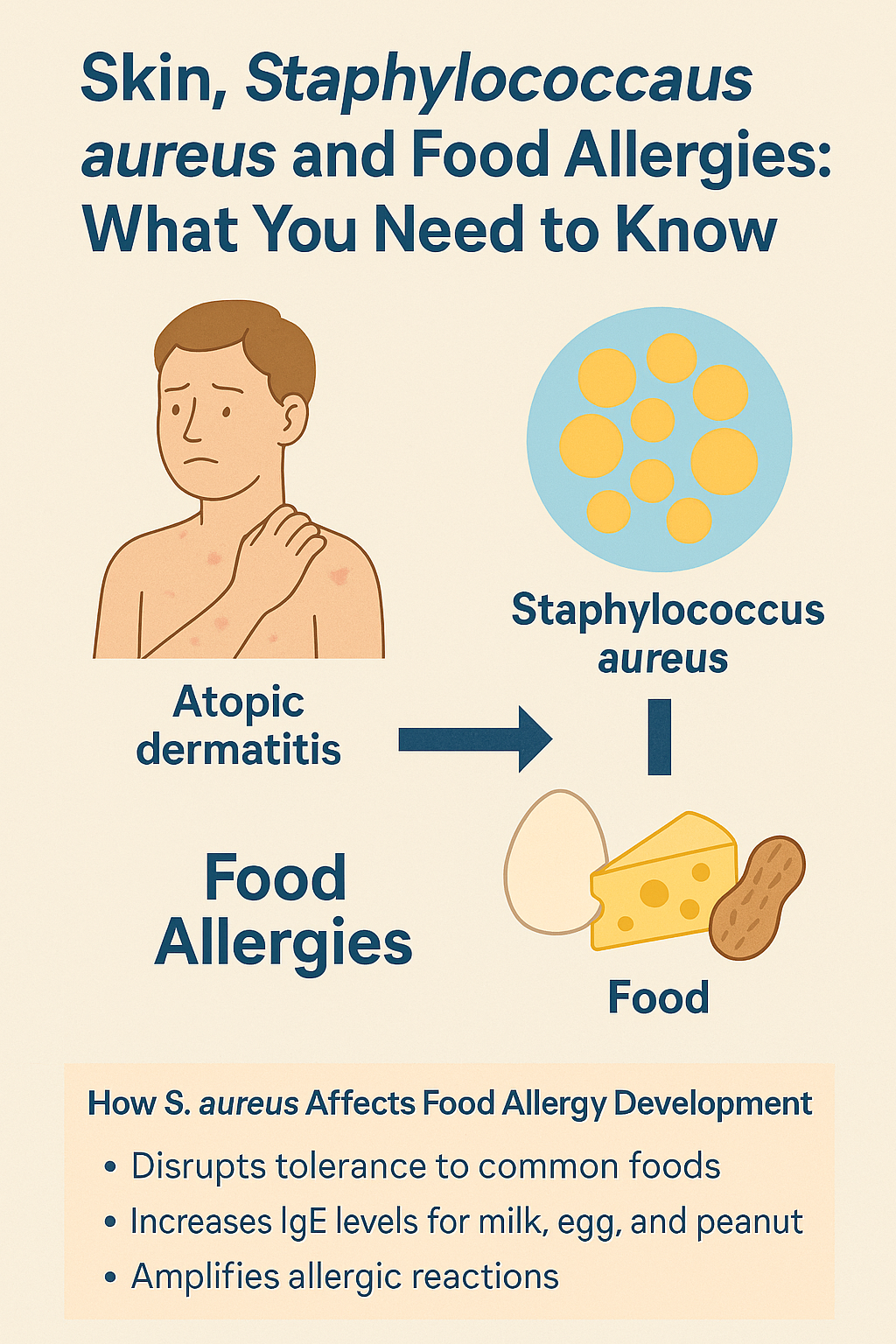
Skin, Staphylococcus aureus, and Food Allergies: What You Need to Know
Atopic dermatitis (AD), commonly known as eczema, is often thought of as a skin condition, but research shows it can have much deeper effects on the immune system. One of the most important (and often overlooked) factors linking eczema to food allergies is a bacterium called Staphylococcus aureus (S. aureus).
Understanding this connection can help explain why children and adults with eczema are at higher risk for developing food allergies—and why early skin care matters more than we once realized.
What Is Staphylococcus aureus?
Staphylococcus aureus is a type of bacteria that commonly lives on the skin. In people with healthy skin barriers, it usually exists in balance with other microorganisms.
However, in individuals with atopic dermatitis, the skin barrier is compromised, making it easier for S. aureus to overgrow and dominate the skin microbiome.
This overgrowth doesn’t just worsen eczema symptoms. It can also influence how the immune system responds to foods.
How S. aureus Contributes to Food Allergy Development
Research has shown several key ways S. aureus affects immune tolerance and allergy risk:
1. Disrupts Food Tolerance
S. aureus on the skin has been shown to interfere with the body’s ability to develop tolerance to common foods such as:
Hen’s egg
Peanut
Instead of learning to recognize these foods as harmless, the immune system may begin treating them as threats.
2. Increases IgE Antibodies
Children and adults with S. aureus colonization may have higher IgE levels—the antibodies associated with allergic reactions to:
Cow’s milk
Hen’s egg
Peanut
Importantly, this can occur even when eczema appears mild, meaning visible skin severity doesn’t always reflect immune risk.
3. Amplifies Immune Reactions
S. aureus produces toxins such as Staphylococcal enterotoxin B, which act as powerful immune stimulants. These toxins can:
Intensify allergic inflammation
Push the immune system toward allergic sensitization rather than tolerance
Why This Connection Matters - Especially in Children
When S. aureus colonizes eczema-prone skin, it doesn’t just cause irritation—it can set the stage for food allergies by disrupting the normal immune education process.
This is especially important in infants and young children, where early immune experiences shape long-term allergy risk.
Managing eczema early and effectively may help:
Support skin barrier repair
Reduce bacterial overgrowth
Lower the risk of developing food allergies
The Takeaway
Eczema isn’t just a skin issue—it’s an immune signal.
Healthy skin plays a critical role in teaching the immune system what is safe. When that barrier is disrupted and bacteria like S. aureus take over, the risk of food allergy increases.
This growing body of research highlights why early, comprehensive eczema management is so important—not just for comfort, but for long-term immune health.
If you or your child struggle with eczema and food reactions, a root-cause, immune-focused approach can make a meaningful difference.
👉 Book your appointment. Link in bio. Or call (949) 239-4000